In a presentation to the American Association for Justice, Shana De Caro discusses falls – the leading cause of traumatic brain injury in the United States.
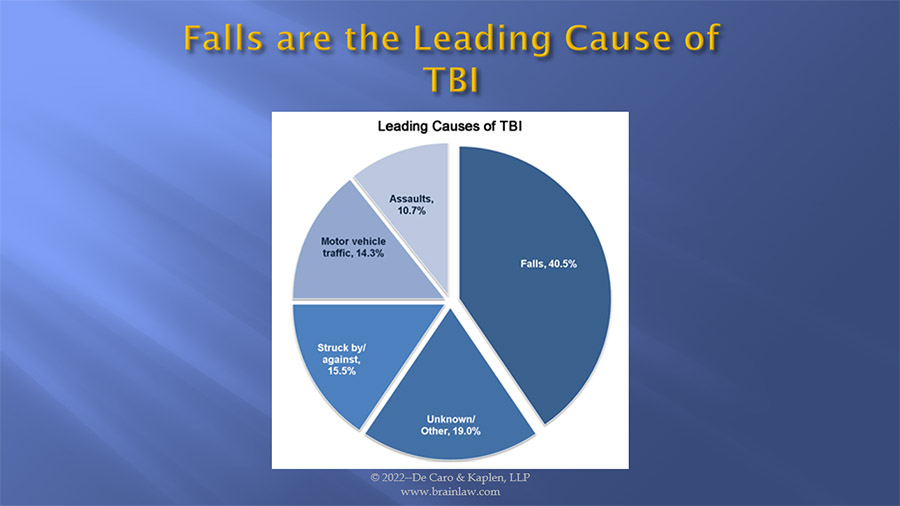
Falls are the leading cause of traumatic brain injuries in the United States, and account for over 40 percent of all TBI’s resulting in an emergency department visit, hospitalization, or death. Falls cause more than half of children’s TBI’s and more than two-thirds of TBI’s in adults over the age of 65. The CDC reports that falls represent the second leading cause of TBI-related death.
Many falls are preventable if proper precautions are taken. Below, I would like to review how the brain is injured in a fall, fall prevention, and legal responsibility, in the context of hospitals, nursing homes, construction sites, sidewalks, and walkways.
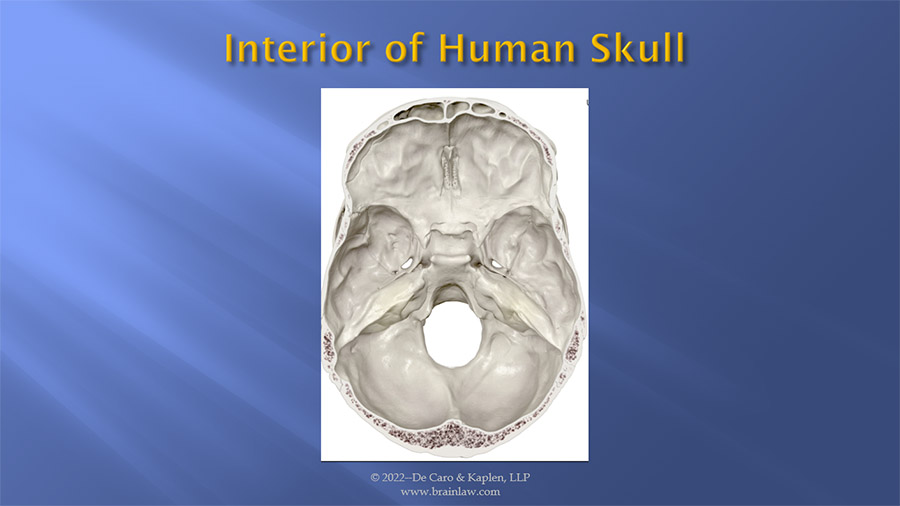
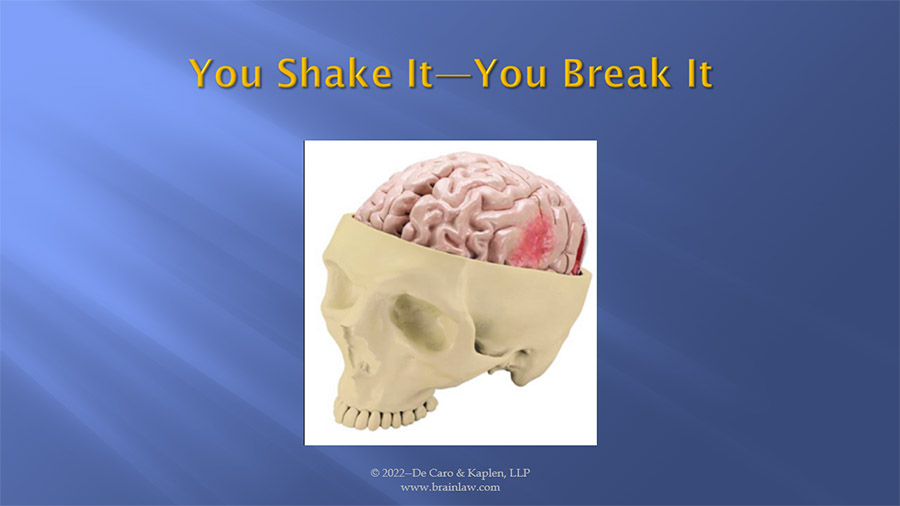
Any discussion of falls, head trauma and resulting brain damage must begin with a review of the skull. While the exterior of the skull may provide protection from penetrating wounds, it is the contours of the interior surface of the skull which contributes to many brain injuries. As you can see from this illustration, the interior surface of the skull has many sharp ridges and protrusions which cause damage to the brain floating in a layer of cerebral spinal fluid within the skull. As the brain moves within the skull as a result of trauma, these surfaces can and often cause damage to the brain. It is always useful to have a model of the brain and skull with you to illustrate this to a jury through your expert witness and request that the interior model of the skull be passed around to the jury so they can touch and feel these surfaces for themselves.
I like to lead with the theme, You Shake It, You Break It, to describe what happens to the brain as it travels in either a lineal or in a rotational manner as a result of trauma. Always remember it is possible to damage the brain without a direct blow to the head.
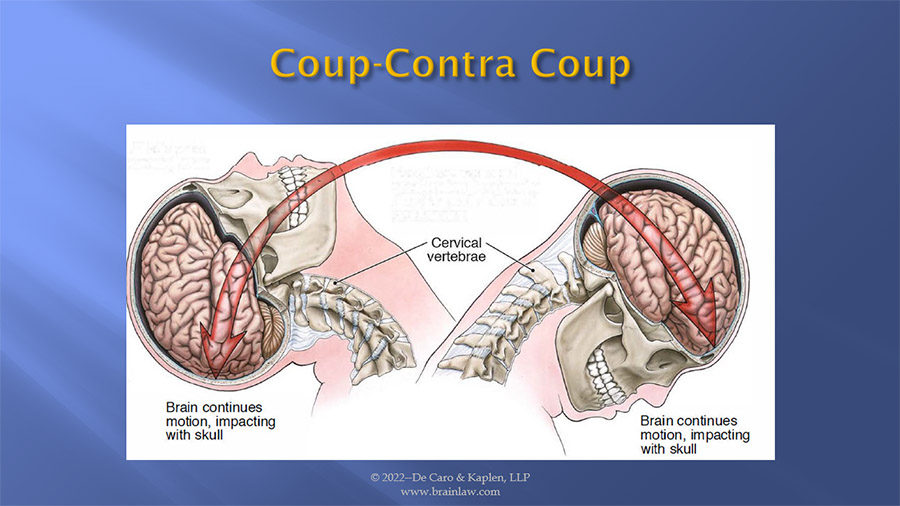
When the brain moves within the skull there are two separate and distinct injuries that take place. The initial injury at the point of contact is called the coup injury, and then when the brain rebounds within the skull a second injury on the opposite side of the brain occurs, known as a contra coup injury. Depending on whether it is the moving brain that strikes a fixed object such as falling on the sidewalk or whether it is a stationary brain that is struck by a moving object (when the head is struck by a falling object while walking on a street) will determine whether the coup or the contra coup injury is greater. When it is the brain that is moving and striking a fixed object, the rebound or contra coup injury is usually the more significant. Alternatively, when a moving object such as a baseball bat strikes the skull, it is the initial injury or coup injury which is the more serious.
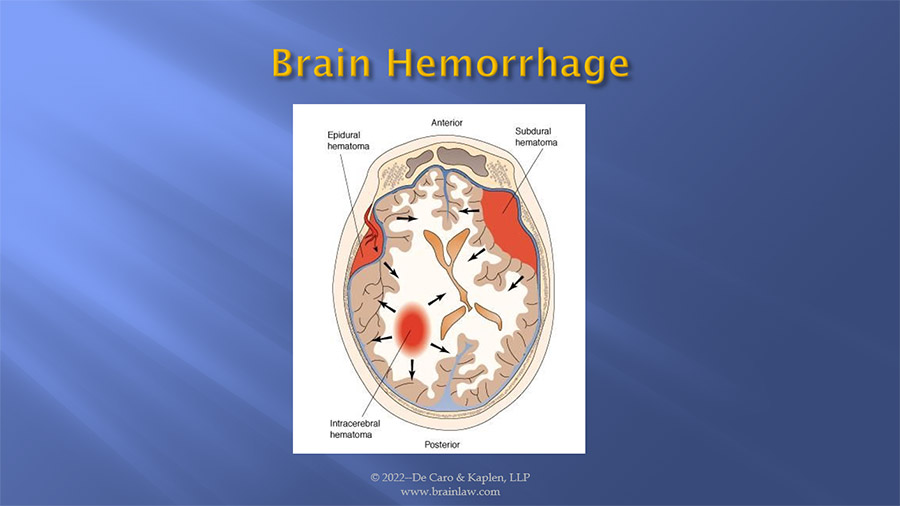
In addition to the physical damage caused to the brain as a result of the initial trauma, secondary injuries occur as a result of bleeding/hemorrhage caused by damage to blood vessels. This bleeding can take place between the brain and the skull known as an epidural hematoma or within the brain itself known as a subdural hematoma. Depending on the size and location of these hemorrhages, they may be evacuated by a neurosurgeons or allowed to remain and the blood becomes reabsorbed within the brain. In either case, the blood will leave a trace substance known as a hemosiderin deposit, an iron deposit that takes place as any remaining blood breakdown. These deposits may be seen on 3 T Tesla MRI studies and are useful to objectively demonstrate brain damage. Bio Mechanical Engineers, forensic pathologists, and neurologists can opine based on this, whether there was sufficient force to cause damage to blood vessels within the brain which can be seen on these scans, and likewise the trauma was sufficient to cause damage to nerve cells which cannot be seen on traditional MRI studies.
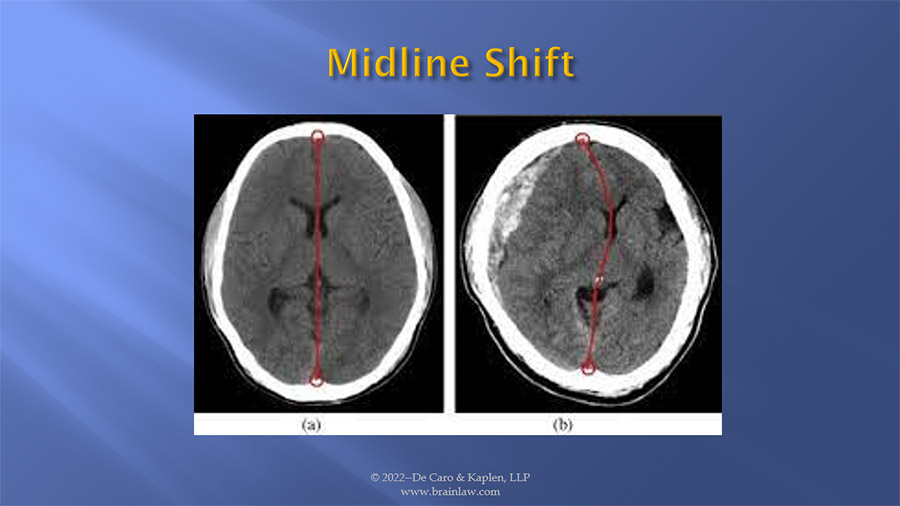
An uninjured brain is symmetrical. The brain is divided along the midline as we see in figure (a). When a hemorrhage occurs, the blood occupies a portion of the space assigned to the brain in the closed skull cavity. The extra blood that is leaking out of broken blood vessels begins to accumulate. This raises overall pressure in the brain, and the growing collection of blood begins to push against brain tissue The brain is then pushed or moved, which is illustrated in image (b). When the brain is pushed from the midline it is referred to as a midline shift which can be seen on a CT image. This brain movement causes trauma to other structures as they are pulled and pushed out of their natural position. The greater the midline shift, the more serious the complications and the greater the risk of death.
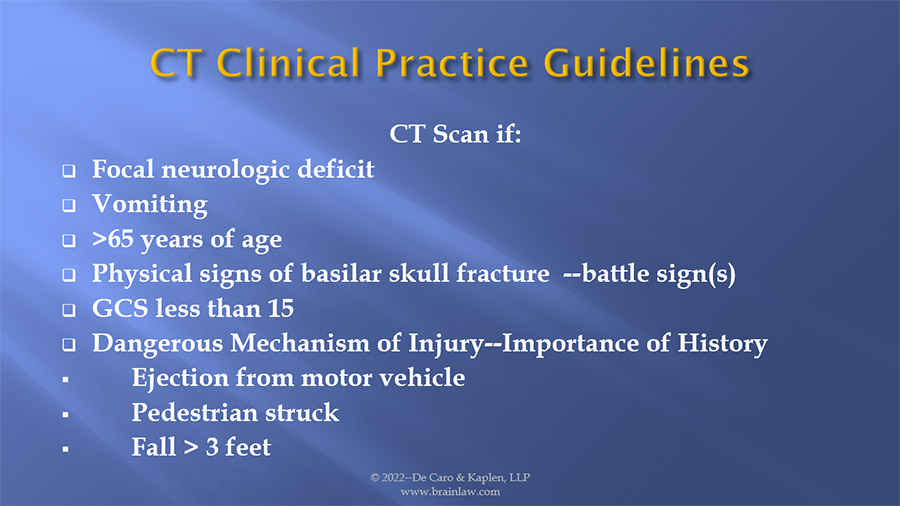
The American College of Emergency Physicians clinical guidelines for the use of CT scans in the emergency department sets forth parameters for the use of a CT. Many of these signs and symptoms are associated with a fall. Any individual with a history of falling greater than 3 feet must always have a CT.
Brain injuries from falls can happen to anyone, anyplace, and anytime. These injuries often are not initially appreciated and can lead to tragic outcomes. The death of actress Natisha Richardson is a good example of a minor fall on a beginner’s ski slope. Ms. Richardson who was skiing with her instructor fell and struck her head. She never lost consciousness, was able to stand after her fall and resume skiing. She initially seemed fine and declined any treatment. Later that night she began to complain of a severe headache. She was rushed to a hospital in an ambulance. She was then transferred to a New York City hospital, where she lapsed into a coma and died two days after the fall. The official cause of her death was epidural hematoma, which is an accumulation of blood between the skull and the thick membrane covering the brain
Rolling Stone legend Keith Richards fell 16 feet from a coconut tree while in Fiji. It was reported that immediately after the fall, Richards felt fine and didn’t feel any serious pain until a few days after when he began complaining of a blinding headache. He was initially diagnosed as suffering a concussion. When further testing was conducted at a hospital, it showed that the guitarist had a subdural hematoma.
It is well-known that falls in hospitals lead to adverse patient outcomes, and prevention of patient falls should be of the utmost importance to all hospital personnel. Falls in hospitals are associated with mortality, morbidity, and reduced ability to function.
Patient falls within hospitals have been identified by The U S Department of Health and Humans Services, Centers for Medicare and Medicaid Services (“CMS”) as “Never Events.”
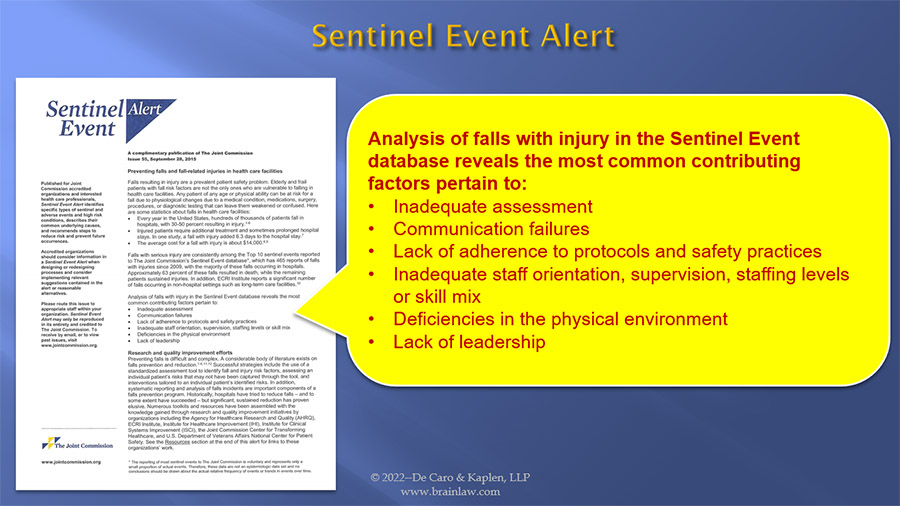
A “Never Event” is an error in medical care that is clearly identifiable, preventable, and serious in its consequences for patients, and indicates an actual and tangible problem within the safety requirements of a health care facility and affects the ability to provide a safe environment and adequate care. The Joint Commission on Accreditation of Hospitals (“JCAHO”) has declared patient falls within hospitals to be “sentinel events” caused by these contributing factors:
A “sentinel event” is defined by JCAHO as a “patient safety event not primarily related to the natural course of the patient’s illness or underlying condition that reaches a patient and results in death, permanent harm, or severe temporary harm where intervention is required to sustain life.”
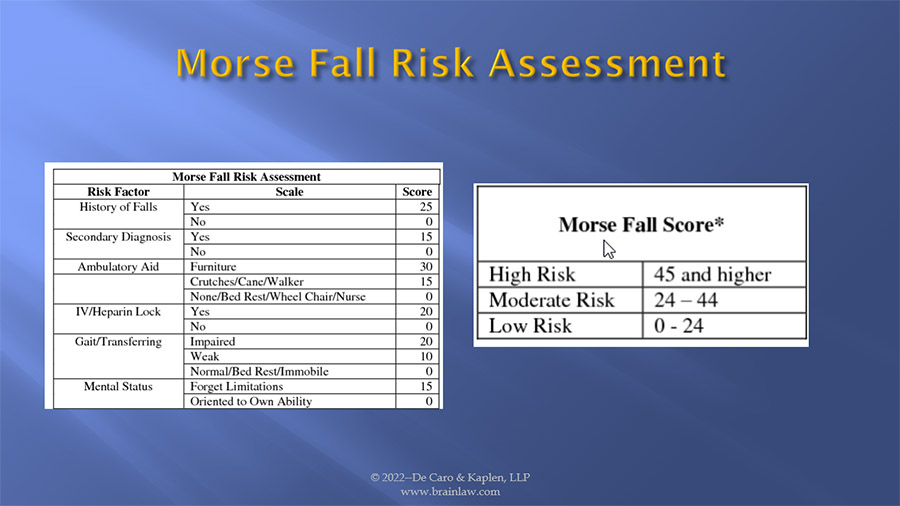
A MORSE FALL SCALE assessment is a tool utilized to gauge a patient’s risk of falling, so that proper and adequate precautions are undertaken and instituted to reduce and/or eliminate the risk of falling. The items in the scale are: History of Falling, Secondary Diagnosis, Ambulatory Aids, Intravenous Therapy, Gait, and Mental Status and each has an associated score. Following the assessment, the score is tallied and recorded on the patient’s chart. Risk level and recommended actions to prevent or reduce the probability of falling is based upon the tallied score. A score of “0-24” is considered “low risk”; a scale of “24-44” is considered a “moderate risk”, and a score greater than “45” is considered a “high risk”. In a recent case, our client presented to the emergency department of a hospital with a urinary tract infection and was found to be disoriented. His wife reported he had fallen several days earlier. A physical examination found he had impaired ambulation. Despite these known fall risk factors, the nursing staff failed to properly assess his fall risk and left him unattended, bed rails down, and without activating any bed alarms or other aids such as video monitoring. He managed to get himself out of bed and began walking. He fell and struck his head resulting in massive brain hemorrhage and injury leading him to require around the clock care. They improperly scored him as a low risk, with catastrophic results. Tragically he just recently passed away from his injuries, after the settlement of his case.
The Agency for Healthcare Research and Quality (AHRQ) is the lead Federal agency charged with improving the safety and quality of healthcare for all Americans. They have developed resources for nursing home facilities both to assess a patient’s fall risk and the prevention measures that should be taken to prevent falls from occurring. The agency reports, approximately half of the 1.6 million nursing home residents in the United States fall each year. A 2014 report by the Office of the Inspector General found that nearly 10% of adverse events experienced by Medicare skilled nursing facility residents were falls resulting in significant injury.
The first step in preventing falls in nursing home is to perform a thorough assessment of a patient’s fall risk, instituting proper interventions, alerting all staff to the patient’s fall risk, and constantly re-evaluating and updating the plan to account for changes in the resident’s condition.
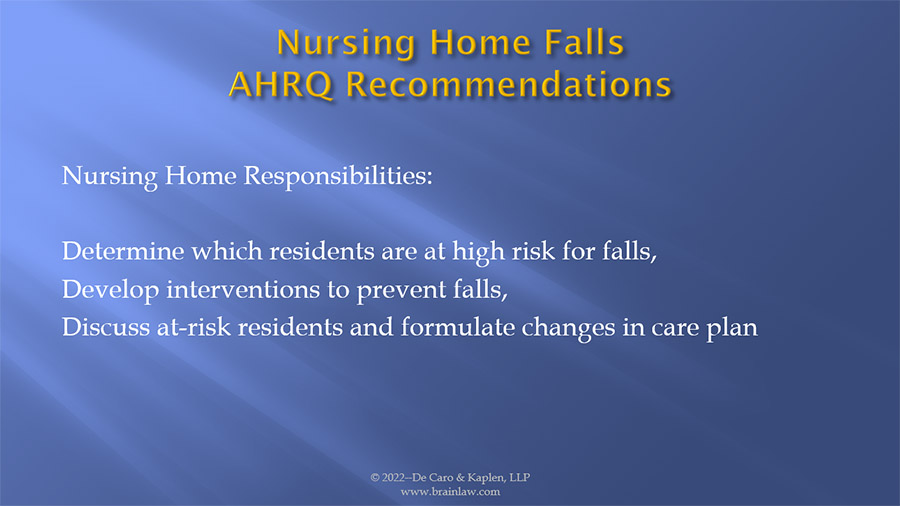
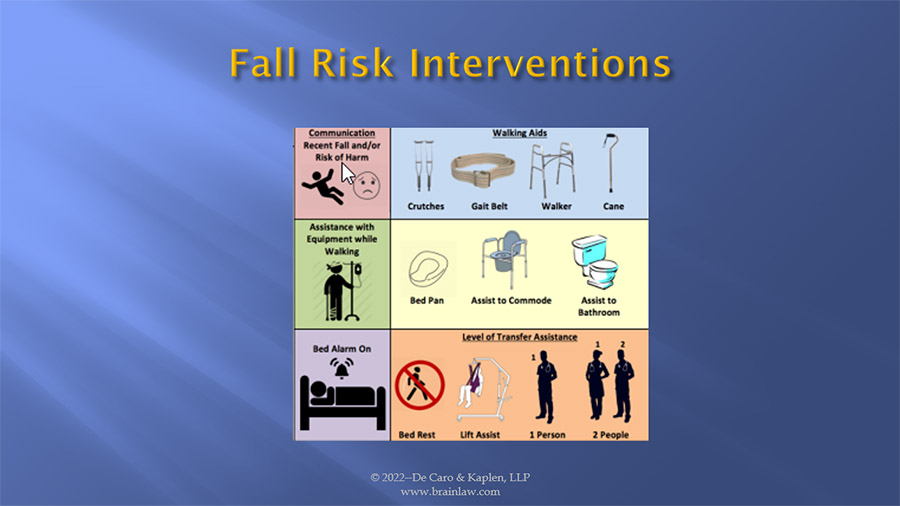
In hospitals and nursing homes, fall risk interventions start with proper assessment of the patient’s risk of falling and communication among staff. Appropriate fall interventions include placing the patient under constant watch and/or surveillance, placing remote visual monitoring at his/her bed side; utilizing bed and/or mattress alarms, and/or bed rails, training staff on how to properly transfer a patient, having sufficient staff, and the availability and use of mobility devices including canes, crutches, and walkers.
AAJ has excellent resources on nursing home fall risk that I recommend you obtain for further information on this topic.
Falls do not just happen in hospitals and nursing homes. Falls are the leading cause of death in construction accidents, accounting for one-third of all construction related fatalities. The construction industry has the greatest number of both fatal and nonfatal traumatic brain injuries among U.S. workplaces. These falls are preventable through proper planning, the use of proper equipment and appropriate employee training. Contractors must determine what proper fall protection measures should be taken in advance of construction activities taking place. Temporary stairways, scaffolds, and aerial lifts need to be provided. Proper equipment including ladders of the proper height and in good repair, personal fall arrest systems with proper anchor points must be provided, along with netting, guardrails installed and maintained, which eliminate holes and provide safe walk surfaces are all important measures. In New York State the Industrial Code enumerates many of these requirements. The Occupational Safety and Health Administration (OSHA) construction regulations are also a valuable reference source.

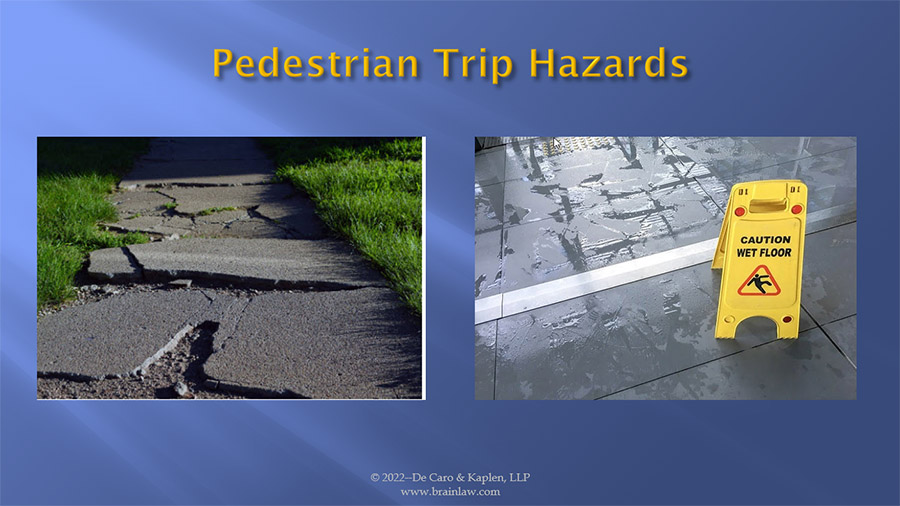
The standard of care for walkways and sidewalks requires property owners and property managers to provide safe walking surfaces. Walking surfaces including stairways, must be properly designed , constructed, and maintained. This responsibility includes proper handrails, stairway risers of proper height and depth, conspicuous landings and tread edges, periodic inspections to identify hazardous conditions and prompt measures to correct hazards. ASTM (Safety Standard F1637) sets forth minimum requirements for safe interior and exterior walkways and sidewalks. The standard requires: Exterior walkways be maintained so as to provide safe walking conditions. Under the standard, exterior walkways can be considered substandard and in need of repair if the pavement is broken, depressed, raised, uneven, or cracked.
Preventing falls following a snow fall requires proper planning. This includes monitoring weather forecasts. You will need a meteorologist to gather weather data, national weather service warnings and advisories to prove notice, temperature conditions and when snow fall stopped. It is vital to determine when snow fall stopped to counter the “snow in progress” defense, which shields defendants from failing to take remedial measures if an accident occurred within a short period of time after the cessation of snow. In NYC, for example, it must be more than 4 hours for liability to attach.
In a recent case we were able to establish the standard of care thorough the pre-trial testimony of the defendant’s employees.
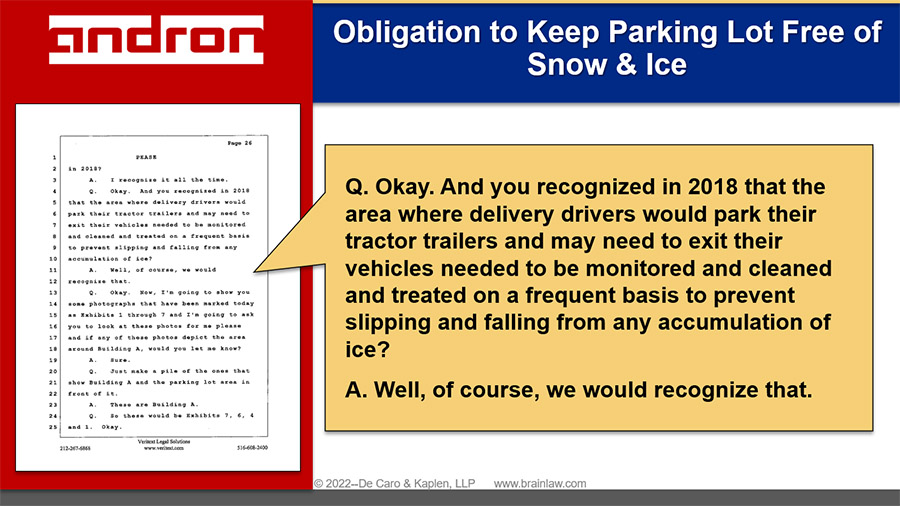
We successfully established the need to monitor weather forecasts and pre-treat areas to prevent the accumulation of ice.
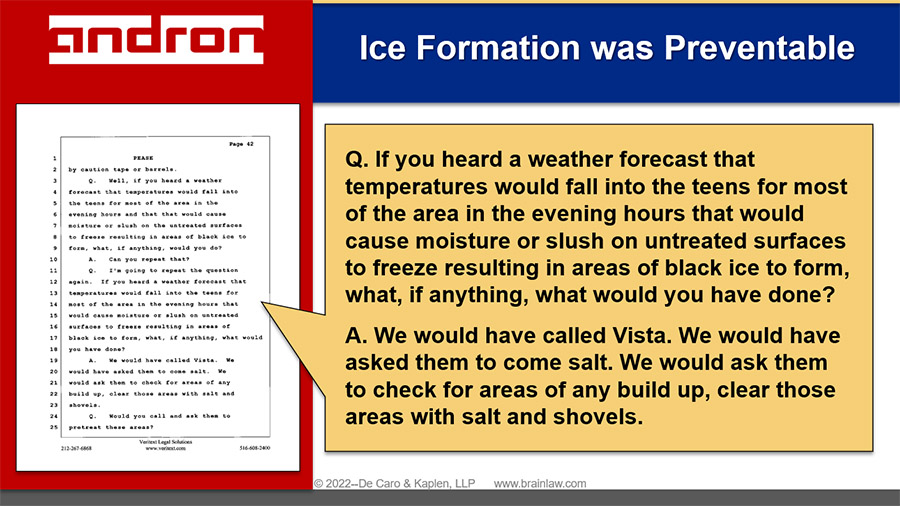
Review of the property owner/manager’s snow removal plan is also an important first step in the prosecution of a snow and ice case. Taking proper measures to prevent the formation of ice when the forecast calls for precipitous drops in temperature is the standard practice. This requires the pre-treatment of surfaces. In evaluating the adequacy of the snow removal response, it is important to determine where snowplows leave the piles of removed snow. Often piles of snow are left in inappropriate locations resulting in melting on the walkway surface and refreezing as temperatures drop.
In this same case we successfully established snow was inappropriately left in piles on the side of the road.
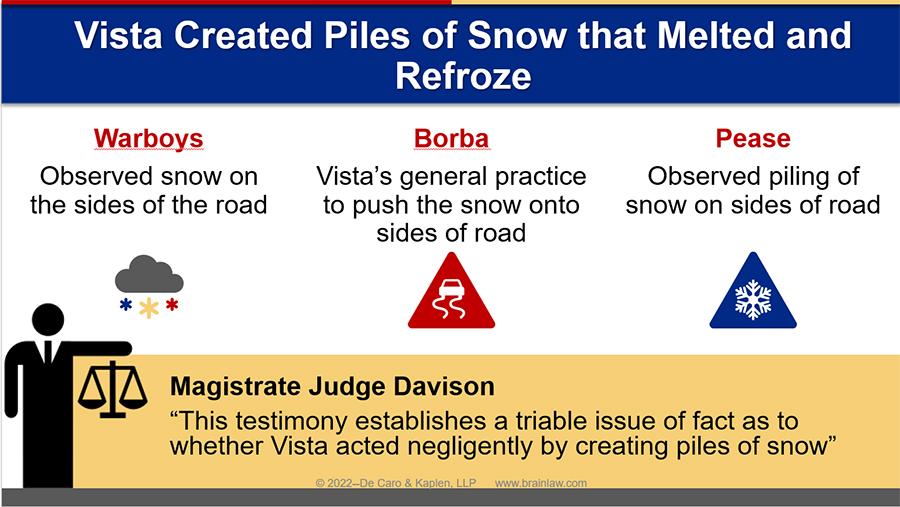
These piles of snow which resulted in melting and refreezing with temperature fluctuations, combined with the failure to provide ice melting chemicals, resulted in the formation of ice causing our client’s fall.
Falls are the leading cause of traumatic brain injury (TBI) for children from 0–4 age years of age. Third-party liability may result from the failure to provide window guards and barriers. Day care facilities, schools, and other custodial environments must supervise young children at all times around fall hazards, such as stairs and playground equipment.
According to the CDC one in four individuals over the age of 65 will sustain a fall each year. Approximately 8% of these individuals visit the emergency department each year because of a fall-related injury. Falls are the most common cause of TBI in older adults. Often traumatic brain injuries are not documented in hospital records because the admission diagnosis was some type of broken bone such as a hip fracture. Senior citizens may be taking blood thinners which increase the risk of bleeding following a fall. Any individual taking a blood thinner should be evaluated by a health care professional following a fall. In many seniors, a brain injury may not be recognized until after the patient is discharged home and can no longer function in the same manner as before the fall and hospitalization. Brain injuries must always be considered when a senior citizen falls.
A fall can happen to anyone, any age, any place, and at any time, and can cause serious brain injuries. Taking proper precautions is essential to preventing falls in all situations. Falls, many times are not unavoidable accidents, but may result from the failure to take preventative measures. The best cure for a brain injury is prevention.
Shana De Caro is the Chairwoman of the Brain Injury Association of America, and a partner in the New York brain injury law firm, De Caro & Kaplen, LLP.